Retinoblastoma or
RB

Retinoblastoma (RB) is a very rare malignant or cancerous tumour of the developing cells of the retina in young children. The retina is the tissue lining the inside of the eye which is made up of nerve receptors that receive the visual information from the outside world . Retinoblastoma is due to the presence of an error or mutation in one of the genes within an immature retinal cell in one or both eyes.
Fortunately retinoblastoma is one of the most curable of all childhood cancers, with over 97% of children surviving in the developed world. In Australia, we see between 20 and 30 cases every year and almost all are in children under the age of five.
Symptoms and Signs of Retinoblastoma
The appearance of a white pupil or leucocoria in a young child, is highly suspicious of RB. Turning of the eye or squint is also suspicious, but fortunately the vast majority of children with a squint do not have RB. Less common forms of presentation include a red eye or the parents may have noticed a deterioration in their child’s vision. Pain is an uncommon sympton and usually the child is otherwise well.
What causes Retinoblastoma
RB is due to the presence of an error or mutation in one of the genes within an immature retinal cell in one or both eyes. In some children the defective gene is inherited from one of the parents, but in most cases we do not know what causes the abnormal gene to develop.

Performing an EUA
Examination Under Anaesthesia
If your eye doctor is suspicious of RB, they will firstly need to perform an examination of your child’s eyes while they are asleep under general anaesthesia (EUA). This involves gently pressing on the eye with a blunt curved instrument so that the entire retina can be viewed with a special high power lens called an ophthalmoscope.
Performing an EUA
The EUA will allow the doctor to ensure that the diagnosis is correct and to establish whether the disease is present in one or both eyes. An ultrasound of your child’s eyes will also be performed at the same time to help confirm the diagnosis and asess the size of any tumours present . This is harmless to your child’s eye and will not cause any discomfort after the operation.
Although the tumour cell type is the same in all forms of retinoblastoma, treatment can vary dramatically depending on whether the condition affects one or both eyes. The results of the EUA will reveal the presence of RB in one or both eyes:
If the disease is confined to the one eye and there is no family history of RB, then the condition is known as “Unilateral Sporadic RB”.
If the disease is present in both eyes and there is no family history of RB, then the condtion is known as “Bilateral Sporadic RB”.
If there is a family history of RB, that is, if one of the parents had the disease in their childhood, the condition is known as “Familial RB”.
*Please only follow the appropriate link for further information regarding treatment of the type of RB diagnosed in your child.
Treatment of Retinoblastoma
The most important aim of treatment is to preserve the life of your child. Saving the eye and preserving vision is also extremely important, but not if it endangers the life of your child. Finally,in achieving these aims, we always try to use treatments which offer the least possible chance of side effects and further risks to your child.
There are a variety of different methods available for treating RB. The method(s) used depend on the number, size and location of the tumours, whether the tumours are present in one or both eyes, and whether there is potential for vision.
The decision as to the most appropriate course of treatment for your child will be made by your eye doctor and the risks and benefits of the various options will be discussed in detail with you prior to commencing any treatment. Most of these treatments are outlined in the sections on Unilateral and Bilateral RB.
Enucleation
For children who need to have removal or enucleation of an eye, I have included a page outlining the details of the operation and what parents can expect after the operation. Parents will be able to see, for example, what their child’s eye will look like at a number of stages following the operation. Please go to “Enucleation” for further information regarding enucleation.
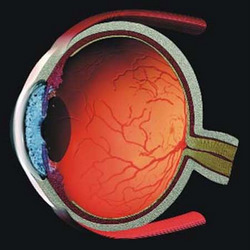
Anatomy of the Eye
Gene Testing
Testing for the mutation in the gene which causes RB is available through the “Institute of Medical and Veterinary Science” in Adelaide, Australia. Please go to “Gene Testing” for further information regarding the genetic basis of RB and the very important role of gene testing.
Metastatic Disease
On rare occasions, tumour cells can escape from the eye and settle in other parts of the body, giving rise to secondary or metastatic disease. This occurs in patients with advanced RB in one or both eyes, and is usually only seen within the first two years from the time of diagnosis. The most common sites of secondary spread include the bones, the meninges (the membrane which covers the brain and spinal cord), the lungs and the liver. The treatment of metastatic RB includes intensive chemotherapy and will be discussed in detail with you by your child’s paediatric oncologist.
Second Malignant Tumours
Second malignant tumours may develop on rare occasions in patients with the heritable or genetic form of RB, that is, Bilateral or Familial RB. The most common second tumours in children include osteosarcoma, which may develop in the bones of the leg or in the bones of the orbit around the eye,and soft tissue sarcomas, which may develop in the muscles of the face or abdomen.
These tumours do not usually develop until many years after the initial diagnosis of RB. Children with the heritable form of RB will require ongoing review by their paediatric oncologist throughout their childhood and teen years. Any unusual symptoms should be immediately reported to their doctor.
Adults who had the heritable form of RB are at higher risk of a number of adult cancers such as breast, lung and skin cancer (melanoma) and should avoid the known risk factors such as smoking and excessive sun exposure. A yearly visit to their local general practioner would be advisable.
